Dysautonomia is an invisible illness that disrupts the autonomic nervous system, affecting millions worldwide. Proper knowledge about its causes, symptoms, diagnosis, and management options will help in better understanding and cure.

Invisible illnesses are conditions that significantly affect a person’s quality of life but are not immediately apparent to others. One such illness that is silently impacting millions worldwide is dysautonomia. This disorder of the autonomic nervous system (ANS) affects critical bodily functions like heart rate, blood pressure, digestion, and temperature regulation. The complexity of dysautonomia, combined with its often misunderstood nature, makes it a challenging and isolating condition for those who suffer from it.
In this blog, we’ll dive deep into the world of dysautonomia, exploring its causes, symptoms, diagnosis, and management options while bringing to light how this invisible illness affects millions globally.
What Is Dysautonomia?
Dysautonomia refers to a range of medical conditions that affect the autonomic nervous system. The autonomic nervous system controls the involuntary functions of the body, including heart rate, blood pressure, digestion, and body temperature. When these functions are disrupted, it can lead to a variety of symptoms that significantly affect daily life.
There are multiple forms of dysautonomia, but the two most commonly discussed are:
- Postural Orthostatic Tachycardia Syndrome (POTS): A condition characterized by an abnormal increase in heart rate when transitioning from lying down to standing up.
- Neurocardiogenic Syncope (NCS): A condition that leads to fainting due to a sudden drop in blood pressure and heart rate.
The Prevalence of Dysautonomia: Millions Affected Globally
Dysautonomia affects millions of people worldwide, but due to its often subtle and varied symptoms, it is frequently misdiagnosed or goes unrecognized for years. Recent estimates suggest that over 70 million people globally may be affected by some form of dysautonomia. This staggering number highlights the need for greater awareness, research, and support for individuals living with this invisible illness.
One of the most common misconceptions about dysautonomia is that it’s rare. In reality, many people with conditions such as diabetes, multiple sclerosis, Parkinson’s disease, and Ehlers-Danlos syndrome are more prone to developing dysautonomia as a secondary disorder.
Common Symptoms of Dysautonomia
Dysautonomia presents a broad range of symptoms, many of which vary from person to person. This is one reason why it’s often referred to as an “invisible illness.” The symptoms are not always visible to others, but they can significantly impact an individual’s day-to-day life. Here are some of the most common symptoms of dysautonomia:
- Chronic Fatigue: Persistent exhaustion that does not improve with rest.
- Dizziness and Fainting: Frequent feelings of lightheadedness, especially when standing up (orthostatic intolerance).
- Irregular Heart Rate: Tachycardia or bradycardia, particularly in response to changes in position.
- Digestive Issues: Such as bloating, nausea, gastroparesis, and constipation.
- Temperature Dysregulation: Trouble controlling body temperature, including heat intolerance or excessive sweating.
- Brain Fog: Cognitive difficulties, such as memory problems, difficulty concentrating, and mental fatigue.
- Anxiety and Depression: Often secondary to the condition, due to the physical and emotional toll it takes on the body and mind.

What Causes Dysautonomia?
The causes of dysautonomia can be as varied as the symptoms, with some forms of the condition being hereditary, while others are secondary to other health conditions. Below are some potential causes of dysautonomia:
- Genetic Factors: Certain inherited conditions, such as familial dysautonomia, are caused by genetic mutations.
- Chronic Illnesses: Autoimmune diseases, diabetes, and chronic infections like Lyme disease have been linked to dysautonomia.
- Neurological Conditions: Diseases like Parkinson’s disease, multiple sclerosis, and Guillain-Barré syndrome can lead to autonomic dysfunction.
- Physical Trauma or Injury: Spinal cord injuries, brain trauma, or surgeries affecting the nervous system can contribute to the development of dysautonomia.
In some cases, the exact cause of dysautonomia remains unknown, making it even more difficult to treat.
Diagnosing Dysautonomia: Why It’s So Challenging
One of the biggest hurdles for individuals suffering from dysautonomia is receiving an accurate diagnosis. The symptoms of dysautonomia overlap with many other conditions, and because it affects so many different bodily functions, it often requires a multidisciplinary approach to identify.
To diagnose dysautonomia, healthcare providers may use several tests, including:
- Tilt Table Test: This test measures how the body responds to changes in position, particularly heart rate and blood pressure.
- Autonomic Function Tests: These evaluate how the autonomic nervous system is functioning, including heart rate variability and sweat tests.
- Blood Pressure Monitoring: Continuous or episodic monitoring to track blood pressure changes in different positions.
Given the complexity of the condition, it’s not uncommon for patients to see multiple specialists before receiving a diagnosis. Often, it’s not until other conditions have been ruled out that dysautonomia is considered.
Managing Dysautonomia: Treatment and Coping Strategies
While there is currently no cure for dysautonomia, there are several ways to manage the symptoms and improve quality of life. Treatment often involves a combination of lifestyle changes, medications, and therapies tailored to the individual’s specific symptoms. Here are some common strategies for managing dysautonomia:
Medications
- Beta-blockers: These can help control heart rate and reduce symptoms of tachycardia.
- Fludrocortisone: Helps the body retain sodium and water, aiding in blood pressure regulation.
- Midodrine: A medication that helps constrict blood vessels and raise blood pressure.
Diet and Hydration
- Increased Fluid Intake: Staying hydrated is crucial, especially for individuals with orthostatic intolerance. Electrolyte-rich drinks can help maintain blood pressure.
- Salt Intake: Consuming more salt can help boost blood pressure in people with low blood pressure issues.
Physical Activity
- Exercise Programs: Low-impact exercises such as swimming, yoga, and cycling can help improve circulation and strengthen the body without exacerbating symptoms.
Compression Garments
- Wearing compression stockings or abdominal binders can help improve blood circulation and reduce the risk of dizziness and fainting.
Cognitive Behavioral Therapy (CBT)
- For many, the mental and emotional toll of living with dysautonomia is significant. CBT can help individuals develop coping mechanisms and manage anxiety and depression associated with the condition.
Living with Dysautonomia: Real-Life Experiences
For many people with dysautonomia, the journey to diagnosis and effective treatment can be long and frustrating. The invisible nature of the illness means that many sufferers are often misunderstood or dismissed by others, including healthcare professionals. Raising awareness about the condition and its effects is crucial for ensuring better support and resources for those affected.
A key aspect of living with dysautonomia is self-advocacy. Many patients have become active participants in managing their own care, seeking out specialists, and educating others about their condition. Online communities, support groups, and organizations such as Dysautonomia International provide valuable resources and a sense of solidarity for those living with the condition.
Dysautonomia: Raising Awareness for an Invisible Illness
Dysautonomia is a complex and often misunderstood condition that affects millions of people around the world. As awareness of the condition grows, so too does the hope for better diagnostic tools, treatments, and ultimately a cure.
Whether you are living with dysautonomia, know someone who is, or simply want to learn more about this invisible illness, understanding the challenges it presents is the first step towards providing better support and care. It’s time to bring dysautonomia out of the shadows and give it the attention it deserves.
Read Next:
The Psychology of Love: Why Valentines Day Matters More Epic Than You Think
Discover the psychology of love and why Valentines Day is more important than you think. Learn how love impacts the brain, strengthens relationships, and boosts

Premier League Highlights: Arsenal Humiliate Man City 5-1, Spurs and Palace Secure Crucial Wins
Arsenal demolished Manchester City 5-1 in a statement premier league highlights win, reigniting their title hopes. Meanwhile, Crystal Palace stunned Man United 2-0, and Tottenham

How Budget 2025 Impacts the Indian Middle-Class: Major Tax Benefits and Glaring Omissions
Budget 2025 offers major tax relief to the middle class, including zero tax on incomes up to ₹12 lakh. However, it misses out on incentives

Degrees vs Employability: Why “Highly Qualified Degree Holders” Struggle to Find Jobs While “Less Qualified Individuals” Get Hired Faster!
Many highly qualified individuals struggle to secure jobs, while less qualified candidates get hired quickly. This Degrees vs Employability paradox is caused by employer preferences,

The Power of Mindset: Why Looking Poor Doesn’t Make You Poor, but Thinking Poor Does!
Discover why looking poor doesn’t define your wealth but thinking poor does. Learn the power of mindset and how a growth-oriented mindset can lead to

Overthinking: How It’s Damaging Today’s Youth – Causes and Cure in 2025
Understanding how overthinking is silently damaging today’s youth, from its causes rooted in societal pressure and social media to its long-term effects on mental health.

Netaji Subhash Chandra Bose: An Epitome of Epic Leadership
Discovering the incredible life of Netaji Subhash Chandra Bose, a leader whose vision, courage, and determination redefined India’s freedom struggle. Explore his leadership qualities, ideology,

Global News Headlines Today: From Gaza Ceasefire to Blue Origin’s Massive 2025 Milestone
Explore today’s top global news headlines, from the Gaza ceasefire and Blue Origin’s historic spaceflight to Apple losing its top spot in China’s smartphone market.

The Hidden Danger of Social Media Nudity: A Threat to Today’s Youth in 2025
Understanding how social media nudity is impacting the youth and their future potential. Learn about the risks of unregulated content, cultural sensitivities, and solutions for

FA Cup 2024: Manchester United Survive Arsenal Test to Advance in FA Cup Fourth Round
Manchester United defeated Arsenal in a thrilling FA Cup third-round encounter, with Atlay Bayindir’s heroics sealing the win. Read about key moments, standout performances, and

Supercopa de España: Barcelona Dominate Real Madrid 5-2 to Claim Supercup
Barcelona delivered a stunning 5-2 victory over Real Madrid in the Supercopa de España final. Read about the key moments, star players, and the significance
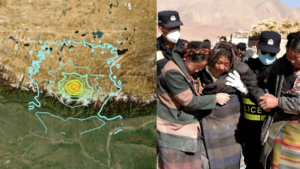
Global News Highlights Today: India’s Metro Milestone, US Aid Shift, iOS Stunning Updates and More!
Explore today’s global news highlights, including the Tibet earthquake, political tensions in South Korea, LA wildfires, US aid shifts, and India’s metro milestone. Stay informed

The Power of Keeping Plans Private in 2025: Why Silence is the Key to Achieving Your Dreams!
Discover why keeping plans private is crucial for achieving your dreams. Learn how silence boosts focus, protects momentum, and helps you achieve success without distractions

Rolls-Royce Ghost Series II Arrives in India 2025: Elegance Meets Stunning Innovation
Discover the all-new Rolls-Royce Ghost Series II launched in India, priced from ₹8.95 crore. Explore its stunning design, luxurious interior, enhanced tech features, and powerful

Global News Highlights: Earthquakes in Tibet, US Bird Flu Crisis Fatality, Brics Welcomes Indonesia in 2025, and Many more
Explore this week’s global news highlights, including the first bird flu death in the US, Indonesia joining Brics, devastating earthquakes in Tibet, rising HMPV cases
